Introduction
Chemotherapy is a dynamic, complex process involving cross-functional healthcare teams and comprises dosing, scheduling, safety checks, compounding and administration. Coupled with team silos, legacy systems, escalating workload and cost, efficient chemotherapy delivery is increasingly challenging, resulting in negative staff and patient experience. A design thinking methodology focused on end-users is ideal for addressing complex problems with no clear best practices.
Aim
We hypothesized that a multidisciplinary team using a data-driven, design thinking approach to redesign chemotherapy workflows can reduce time to treatment, improve operational efficiency and staff and patient experience.
Methods
A process mapping exercise was undertaken to understand the chemotherapy process. Patients and staff from different job groups were shadowed. The problem statement was "60% of patients are waiting more than an hour from their appointment time to start treatment". The following examples of "how might we" questions were used for the ideation phase:
1. How might we increase advanced chemotherapy preparations (premakes) for patients?
2. How might we ensure only premakes are listed in the mornings?
Separately, we also designed an anonymized database to track chemotherapy delivery and care provision outcomes by writing an algorithm to link data extracted from appointment, queue management and chemotherapy systems. New workflows were drafted, iterated, and implemented from 1 May 2020 with the following major changes:
1. No same day blood tests and chemotherapy, with physicians reminded to complete chemotherapy orders by 3pm the day before to allow advance compounding.
2. All chemotherapy regimens were consolidated into a directory containing properties like infusion duration, premake eligibility (based on drug stability and cost) and other scheduling characteristics. This was made searchable via an Excel (Microsoft, USA) algorithm, which also recommended ideal booking slots for the scheduling team. Premakes were prioritized for morning (0830 - 1030) slots.
3. Outcome targets were agreed on and tracked daily. These were made accessible to all staff via a dashboard. The workgroup met weekly to discuss targets, barriers and iterate workflows. Daily, intra-group communication was facilitated by TigerConnect (TigerConnect, USA).
We included consecutive outpatients treated at our institution from 1 Jan - 27 Jul 2020. Patients were split into two groups: a historical control group (1 Jan - 30 Apr) and a post-intervention study group (1 May - 27 Jul).
The primary outcome measure was the difference between appointment time and time treatment started. Secondary outcome measures included (a) proportion of premade chemotherapy; (b) number of patients starting treatment within an hour of appointment time; and (c) number of patients finishing treatment after 6pm.
Continuous data are reported as median (25th-75th centile) and analysed with the Mann-Whitney U test, while categorical data were assessed with the chi-square test. Analysis was done with SPSS v22 (IBM, USA).
Results
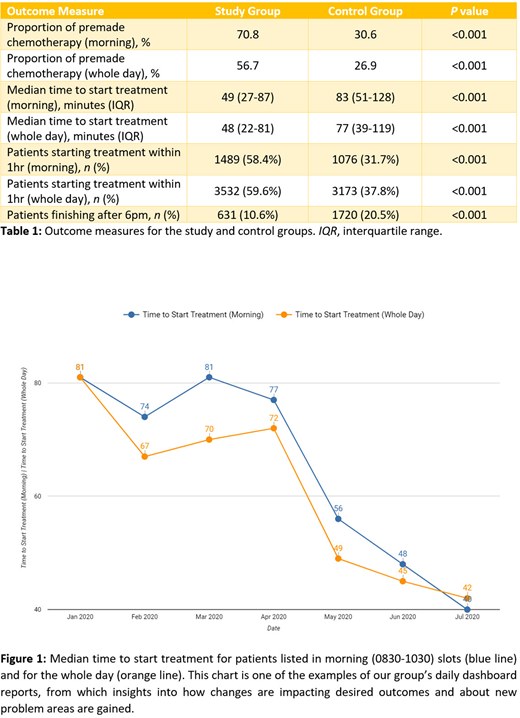
Results are summarized in Table 1. From 1 Jan - 27 July 2020, 14314 treatments were completed. Of these, 5946 (41.5%) were in the 0830 - 1030 slots prioritized for premade chemotherapy. 18.8% of patients arrived after their appointment time. The proportion of premade chemotherapy increased to 70.8% from 30.6% (p<0.001).
The median time to start treatment decreased from 83 (51-128) minutes in the control to 49 (27-87) minutes in the study group (p<0.001). This translated into an improvement for the day overall (Figure 1).
The proportion of patients with morning appointments starting treatment within 1 hour of their appointment time increased to 58.4% from 31.7% (p<0.001). For the whole day, this increased to 59.6% from 37.8% (p<0.001), resulting in less patients finishing treatment after 6pm (20.5% to 10.6%, p<0.001).
Conclusion
We have shown that a multidisciplinary group using a data-driven, design thinking approach to address team silos, reorganize and track work processes can improve the time taken to start treatment. Changes were made at no added cost to the healthcare system and using accessible software. Potential cost savings in terms of less overtime claims for staff have yet to be factored in. Addressing patient punctuality and registration and triage processes will help further decrease time to treatment.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.